Semaglutide, a medication used primarily for the management of type 2 diabetes, has garnered significant attention in recent years due to its efficacy and unique mechanism of action. Understanding the nuances of semaglutide, including dosage, potential side effects, and its broader implications in diabetes management, is crucial for both patients and healthcare professionals alike.
What is Semaglutide?
Semaglutide belongs to a class of medications known as glucagon-like peptide-1 receptor agonists (GLP-1 RAs). It mimics the action of the natural hormone GLP-1, which is involved in the regulation of blood sugar levels. By activating GLP-1 receptors, semaglutide helps stimulate insulin release, suppresses glucagon secretion (which reduces blood sugar), and slows down gastric emptying, leading to improved blood glucose control.
Dosage and Administration
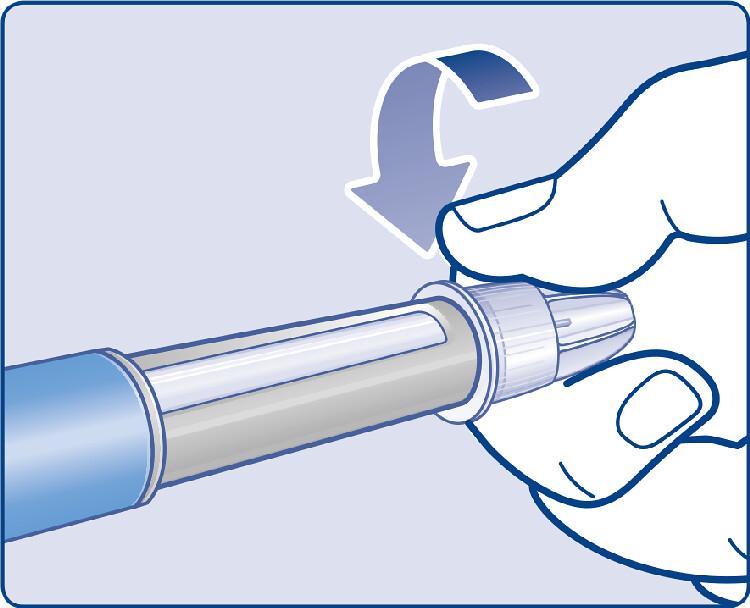
One of the notable aspects of semaglutide is its once-weekly dosing regimen, which offers convenience and potentially improves patient adherence compared to daily dosing regimens of other medications. The standard starting dose of semaglutide is typically 0.25 mg once weekly, with the option to increase to 0.5 mg and then to 1 mg if additional glycemic control is needed. The medication is administered via semaglutide injection injection and can be self-administered by patients after proper training.
Efficacy in Glycemic Control
Clinical trials have demonstrated the efficacy of semaglutide in reducing HbA1c levels, a key marker of long-term glucose control. Studies have shown that semaglutide can lead to significant reductions in HbA1c levels, often surpassing those achieved with other antidiabetic medications. Additionally, semaglutide has been associated with weight loss, making it a particularly attractive option for patients with type 2 diabetes who struggle with obesity.
Common Side Effects
Like any medication, semaglutide is not without its potential side effects. Common side effects may include nausea, vomiting, diarrhea, and abdominal discomfort, particularly during the initial weeks of treatment. These gastrointestinal symptoms often subside over time as the body adjusts to the medication. However, patients experiencing persistent or severe symptoms should consult their healthcare provider.
Less Common but Serious Side Effects
While rare, semaglutide has been associated with more serious side effects such as pancreatitis and medullary thyroid carcinoma in animal studies. However, the clinical significance of these findings in humans remains uncertain. As with any medication, healthcare providers should carefully weigh the potential risks and benefits of semaglutide before prescribing it to patients, particularly those with a history of pancreatitis or thyroid disorders.
Patient Considerations
Before initiating treatment with semaglutide, healthcare providers should assess patients for factors such as renal function, gastrointestinal disorders, and history of pancreatitis or thyroid disease. Semaglutide may not be suitable for all patients, and alternative treatment options should be considered for those with contraindications or intolerances to the medication.
Future Directions
Beyond its role in glycemic control, semaglutide has shown promise in other areas of medicine. Higher doses of semaglutide have been studied for the treatment of obesity, with notable reductions in body weight observed in clinical trials. Additionally, ongoing research is exploring the potential cardiovascular benefits of semaglutide, including its effects on reducing the risk of cardiovascular events in patients with type 2 diabetes.
Conclusion
Semaglutide represents a valuable addition to the armamentarium of medications available for the management of type 2 diabetes. Its once-weekly dosing regimen, efficacy in glycemic control, and potential for weight loss make it a compelling option for many patients. However, healthcare providers must remain vigilant for potential side effects and carefully assess each patient’s individual risk profile before prescribing semaglutide. With continued research and clinical experience, semaglutide holds promise not only for improving glucose control but also for addressing the broader challenges of obesity and cardiovascular disease in patients with type 2 diabetes.
Top of Form